Military service members often face a myriad of challenges, including the risk of injury and exposure to traumatic events during their service. When military medical care falls short, the consequences can extend beyond physical harm, potentially contributing to the development or exacerbation of Post-Traumatic Stress Disorder (PTSD). In this blog, we explore the complex intersection of military medical malpractice and PTSD, shedding light on the unique challenges faced by service members seeking justice for both physical and psychological injuries.
Understanding Post-Traumatic Stress Disorder (PTSD):
PTSD is a mental health condition that can develop in individuals who have experienced or witnessed traumatic events. Military service members, due to the nature of their profession, may be exposed to events that can trigger PTSD, including combat, injury, or the loss of comrades. When medical malpractice occurs in the context of these events, it can compound the emotional toll and contribute to the development of PTSD.
Trauma and Medical Care:
Service members often seek medical care following traumatic events, both physical and psychological. Military medical providers play a crucial role in addressing both the immediate physical injuries and the potential mental health consequences of trauma. When medical care is negligent or inadequate, it can exacerbate the emotional distress and contribute to the development of PTSD.
Failed Duty of Care and Trust:
Military medical malpractice involves a breach of the duty of care owed to service members. When individuals entrust their well-being to military healthcare providers and that trust is violated through negligent care, the emotional impact can be profound. The breach of this duty can further contribute to the development of PTSD, as service members grapple with the betrayal of the very system designed to care for them.
Delayed or Incorrect Diagnoses:
In cases of medical malpractice, delayed or incorrect diagnoses are not uncommon. When mental health conditions like PTSD are misdiagnosed or overlooked, service members may be denied the timely and appropriate interventions necessary for their recovery. This failure to address mental health needs can compound the trauma and contribute to the persistence of PTSD symptoms.
Contributing Factors to PTSD:
Medical malpractice can contribute to the development of PTSD through various factors, including:
a. Inadequate Pain Management: Failure to manage physical pain appropriately can exacerbate emotional distress and contribute to the development of PTSD.
b. Surgical Errors: Traumatic experiences during surgery, compounded by surgical errors, can contribute to the emotional trauma that underlies PTSD.
c. Medication Errors: Incorrect prescriptions or dosage errors may impact mood regulation and contribute to mental health challenges.
Legal Challenges in Proving PTSD Causation:
Proving causation in cases involving PTSD is inherently complex. Establishing a direct link between medical malpractice and the development of PTSD requires a nuanced understanding of both the legal and psychological aspects. Expert testimony from mental health professionals may be necessary to demonstrate how the malpractice directly contributed to the psychological trauma.
Overlap with Physical Injuries:
In many military medical malpractice cases, physical injuries and PTSD often coexist. Establishing causation becomes even more intricate when attempting to demonstrate how negligent medical care impacted both physical and psychological outcomes. Legal strategies must account for the intricate interplay between these aspects of the case.
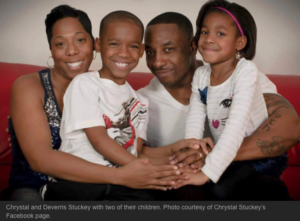
Dual Impact on the Individual and Family:
The intersection of military medical malpractice and PTSD doesn’t only affect the service member; it has a profound impact on their families as well. The emotional toll extends to the relationships and dynamics within the family unit, requiring comprehensive legal and psychological support for all affected parties.
Legal Advocacy for Comprehensive Compensation:
Legal advocacy in cases involving the intersection of military medical malpractice and PTSD must address the comprehensive impact on the individual’s life. Compensation should account for both the physical and psychological aspects of the injury, ensuring that the affected service member and their family receive the support needed for recovery.
Accessing Mental Health Resources:
Service members dealing with the intersection of military medical malpractice and PTSD should prioritize accessing mental health resources. Seeking therapy, counseling, and support groups can aid in coping with the emotional fallout and contribute to the healing process.
Conclusion:
The intersection of military medical malpractice and PTSD presents a unique set of challenges, both in terms of legal complexities and the profound impact on the lives of service members and their families. Recognizing the interconnected nature of physical and psychological injuries is crucial in building comprehensive legal strategies that address the full scope of the harm suffered. With specialized legal advocacy, mental health support, and a commitment to seeking justice, affected individuals can navigate the complexities of their cases and work towards healing and recovery.

 Call Now- Open 24/7
Call Now- Open 24/7